

At Camelback Spine Care, we are one of the few medical centers that can offer same-day outpatient spinal procedures with the same quality and care provided to more advanced surgical treatments. With the innovations and modern techniques available to select surgeons today, Camelback Spine is proud to offer these treatments that allow the patient to go home the same day the treatment is done! This means getting back to enjoying the life and mobility you deserve. As a leading spine surgery center in Arizona, Camelback Spine Care provides a variety of outpatient spine surgery options, including outpatient spinal procedures for lumbar and cervical conditions. Call Camelback Spine Care today if you feel that these same-day treatment options are right for you.
A laminectomy is typically performed to alleviate pain from lumbar spinal stenosis.
Spinal stenosis is caused by degenerative changes that lead to enlargement of the facet joints in the back of the vertebrae.
The enlarged joints and related degenerative changes place pressure on the nerve roots as they exit the spine.
Each vertebra has two portions of vertebral bone over the nerve roots in the back of the spine. These small, flat bones are called laminae.
The lamina functions as a protective covering of the spinal canal. In the lower back, they protect the cauda equina, the nerve roots that branch off of the spinal cord, as well as the nerve roots as they exit the spine.
Most people report measurable improvement in their symptoms after a laminectomy, particularly a decrease in pain that radiates down the leg or arm. But this benefit may lessen over time if you have a particularly aggressive form of arthritis. Laminectomy is less likely to improve pain in the back itself.
A follow-up appointment with our doctors will provide a better assessment of your procedure, as results can vary from patient to patient.
The Coflex device can be used to treat LSS and is a single-piece titanium implant that is stable, strong, and flexible enough to give your spine the support it needs. It provides spinal stability without the invasiveness and loss of mobility associated with spinal fusion. If you or a loved one is recommended for the Coflex procedure, the spine surgeon may choose to perform the procedure in an outpatient setting where patients can experience better outcomes, lower infection rates, cost savings, and more personalized service. Coflex spine surgery is ideal for patients seeking stability without traditional spinal fusion.
The Coflex procedure can be performed in an outpatient setting. However, you should arrange for someone to drive you and to help during the first few hours of your recovery after surgery.
Decompression surgery involves removing the pressure on the nerves that causes pain. After undergoing decompression surgery, our doctors will insert the Coflex device through the incision made for the decompression. The coflexTM device is positioned on your lamina, which is the strongest bone in the back of your spine. On average, the entire procedure, including decompression and implantation of the Coflex device, usually takes less than 2 hours.
When you wake from recovery, you may be encouraged to get up and walk almost immediately, taking into consideration your overall health at the time of surgery. Since there is no fusion and, therefore, no healing bone to wait for, you’ll most likely be able to do this right after your procedure. You’ll notice that your pain has been significantly relieved, and your spine should feel stable and strong. Most patients do need to wait several days following the surgery for the incision wound to heal.
In the weeks and months following surgery, your recovery depends on a number of factors, including the degree of your stenosis and the extent of the decompression that was performed. Most patients are able to return to normal activity, and even expanded activity such as golf, cycling, or gardening, within weeks of the surgery. Some patients may require physical therapy to help with mobility and flexibility.
Typically performed for a herniated disc, a microdiscectomy relieves the pressure on a spinal nerve root by removing the material causing the pain.
A microdiscectomy is generally considered the gold standard for removing the herniated portion of a disc that is pressing on a nerve, as the procedure has a long history and many spine surgeons have extensive expertise in this approach. A microdiscectomy surgery is generally considered a minimally invasive surgery, as there is minimal disruption of the tissues and structures in the lower back.
A microdiscectomy is performed through a 1 to 1½-inch incision in the midline of the lower back.
First, the back muscles (erector spinae) are lifted off the bony arch (lamina) of the spine and moved to the side. Since these back muscles run vertically, they are held to the side with a retractor during the surgery; they do not need to be cut.
The nerve root is gently moved to the side.
Our surgeons use small instruments to go under the nerve root and remove the fragments of disc material that have extruded from the disc.
In a microdiscectomy, only the small portion of the disc that has herniated or leaked out of the disc is removed; the majority of the disc is left as is. Many patients undergo outpatient microdiscectomy or herniated disc surgery, which is minimally invasive to reduce downtime and improve recovery speed.
The total procedure takes about 1 hour to complete. Patients are generally permitted to go home the same day, but they will be advised by physical and occupational therapists on proper in-home techniques before discharge. Patients should avoid bending too much at the waist and refrain from lifting heavy objects for the first couple of weeks. This, along with proper techniques for getting in and out of bed and using the restroom, will help prevent straining the injury. Additionally, patients should avoid sitting for extended periods during the first couple of weeks after surgery.
Our surgeons may recommend a back brace or a soft lumbar corset to provide additional lumbar support after the procedure. The wound area is left clean and open, with no surgical dressing or bandages required. Patients can return to bathing within a day or two after the procedure, and resuming other routines such as driving and returning to work is typically possible within a few days to a week. Our surgeons will schedule a follow-up appointment about 2 weeks after surgery to assess the progress of recovery.
Spinal cord stimulators are often used for neurostimulation for chronic pain. This spinal cord stimulation surgery is generally performed as an outpatient procedure for eligible patients. Spinal cord stimulators may be used to treat or manage different types of chronic pain, including:
Spinal cord stimulation can improve overall quality of life and sleep, and reduce the need for pain medicines. It is typically used along with other pain management treatments, including medications, exercise, physical therapy, and relaxation methods. Several kinds of spinal cord stimulation systems are available. The units that are more commonly used are fully implanted and have a pulse generator, which is like a battery. Most of the newer devices feature a rechargeable pulse generator system that can be easily charged through the skin. There are also some pulse generators that are fully implanted and do not require recharging, but last a shorter time before they need to be replaced. Another system includes an antenna, a transmitter, and a receiver that relies upon radio frequency to power the device. In these systems, the antenna and transmitter are carried outside the body, while the receiver is implanted inside the body. Spinal cord stimulation is recommended when other treatments have not been successful, when surgery is not likely to help, or when surgery has failed. Spinal cord stimulation, also called neurostimulation, directs mild electrical pulses to interfere with pain messages reaching the brain. A small device implanted near the spine generates these pulses. The implanted generator used in spinal cord stimulation has similarities to a cardiac pacemaker, leading some to call the device a pacemaker for pain.
During spinal cord stimulation, a device that delivers the electrical signals is implanted in the body through a needle placed in the back near the spinal cord. A small incision is then made to place the pulse generator in the upper buttock. The patient may turn the current off and on or adjust the intensity of the signals. Some devices cause what’s described as a pleasant, tingling sensation, while others do not. Research shows that newer devices may change the sensation of pain by potentially altering the balance of cells that deliver pain in the spinal cord. During the permanent implantation procedure, the generator is placed underneath the skin, and the trial electrodes are replaced with sterile electrodes. Unlike the trial electrodes, these will be anchored by sutures to minimize movement. The implantation can take about 1-2 hours and is typically performed as an outpatient procedure.
After administering the local anesthesia, your surgeon will make one incision (typically along your lower abdomen or buttocks) to place the generator, and another incision (along your spine) to insert the permanent electrodes. Each incision is about the length of a credit card. Once the electrodes and generator are connected and functioning, our team will close the incisions.
Generally, the pain relief provided by spinal cord stimulators allows patients to do much more than they could before surgery, but there are certain restrictions to be mindful of.
MRIs are not always safe for those with spinal cord stimulation devices!! Some newer devices are compatible with certain MRI machine models and scan locations, but your doctor will need to evaluate the specifics of your stimulator first. If your device is not MRI compatible, MRIs can cause serious injury. You should power off your stimulator when you’re driving or operating heavy machinery, as sudden changes in stimulation levels could cause distraction. Swimming is fine with a permanent, implanted generator, but you cannot get your temporary stimulator wet. You will need to avoid baths and showers during that short trial period. A spinal cord stimulator can be removed safely if you are unsatisfied with the level of pain relief it provides or if there is an infection or mechanical problem with your system
The natural cervical intervertebral disc is a remarkable mechanical structure from an engineering perspective. It has the ability to absorb a large compressive load while still providing an impressive range of motion between the bones in the neck. Duplicating the natural disc's form and function with an artificial disc is challenging. However, several artificial cervical discs have been developed and are available as a surgical option to treat cervical disc problems that cause chronic neck pain and other symptoms, such as arm pain or weakness. Candidates often benefit from cervical disc replacement surgery with an artificial disc replacement neck, restoring motion while relieving nerve compression.
Before having cervical disc replacement surgery, the surgeon typically requests the following of the patient in the weeks leading up to the procedure:
A single-level cervical ADR surgery commonly involves the following steps:
After cervical artificial disc replacement surgery, most patients go home the same day whereas others spend a night in the hospital. During this short stay in the hospital, the patient receives:
A Kyphoplasty procedure is an outpatient surgical procedure that treats small breaks and fractures in the vertebrae that make up the spine. Without treatment or surgical procedures, these fractures can curve and shorten the spine. This kyphoplasty procedure, also called minimally invasive kyphoplasty, is used for vertebral compression fracture treatment, providing quick pain relief and restoring spinal height.
Our doctors are able to complete this complex procedure, designed to stop the pain caused by a spinal fracture, without the need for a hospital setting. In addition to relieving pain, they will stabilize the bone and restore some of the lost vertebral body height due to compression and spinal fractures. This minimally invasive surgery is performed through a small skin puncture rather than a larger incision and typically takes 1 to 2 hours.
During the kyphoplasty procedure, the back is cleaned and prepped for the placement of the needle to puncture the skin. Local anesthesia and mild sedation are applied, although the patient will remain awake during the procedure. Once the small incision is made in the back, a tube is inserted through the path created in the vertebra and into the fractured area.
A specialized balloon will then be inserted through the tube and into the fractured vertebra to be inflated. The inflated balloon creates a soft inner bone support for the fractured vertebra, allowing it to return to normal height. Once the balloon is removed, the cavity of the damaged vertebra will be filled with a cement-like material that will quickly harden and mimic the natural bone structure.
After a kyphoplasty procedure, our team will monitor the patient in the recovery area for a few hours. If there are no complications, the patient is typically allowed to go home with the assistance of someone. Patients are advised not to drive themselves. While most patients may experience immediate relief, others might notice a gradual reduction in pain over time.
This outpatient procedure allows patients to return to their normal routines almost immediately, but they should be limited to non-strenuous activities for 4 to 6 weeks. Our team will follow up with the patient through a virtual or in-person appointment a few weeks after the procedure to assess their recovery.
WHAT WE OFFER
Neck Pain
LEARN MORE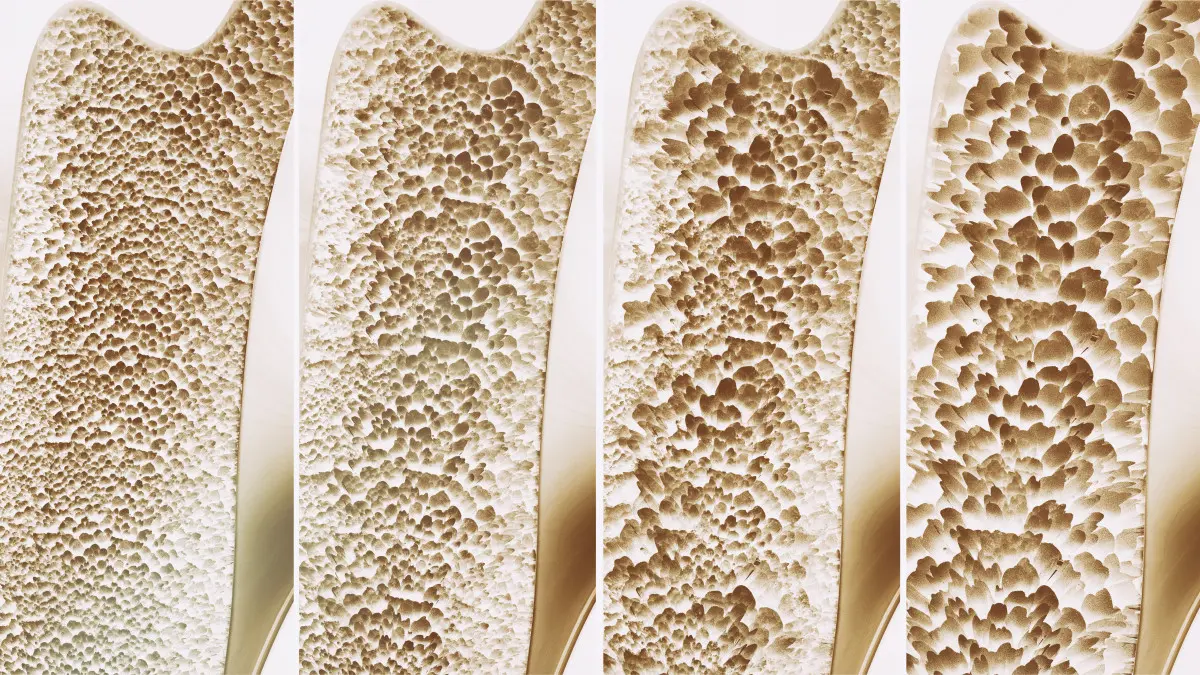
Osteoporosis
LEARN MORE
Lower Back Pain
LEARN MORE
Arthritis
LEARN MORE
Herniated Disc
LEARN MORE
Spinal Stenosis
LEARN MORE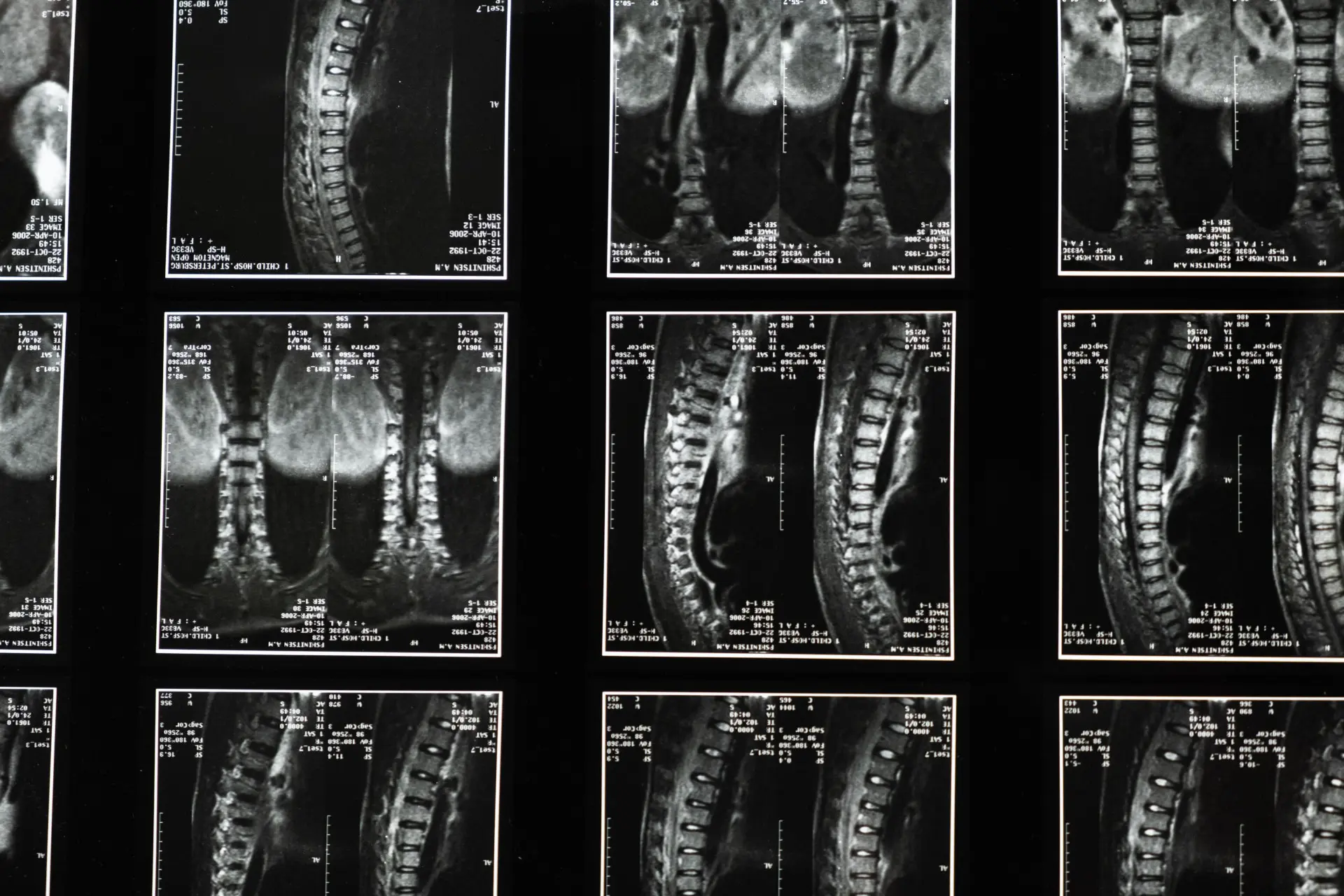
Degenerative Disc
LEARN MORE
Scoliosis
LEARN MORE

